mantle cell lymphoma treatment
 Treatment of mantle cell lymphoma in older adults - Journal of Geriatric Oncology
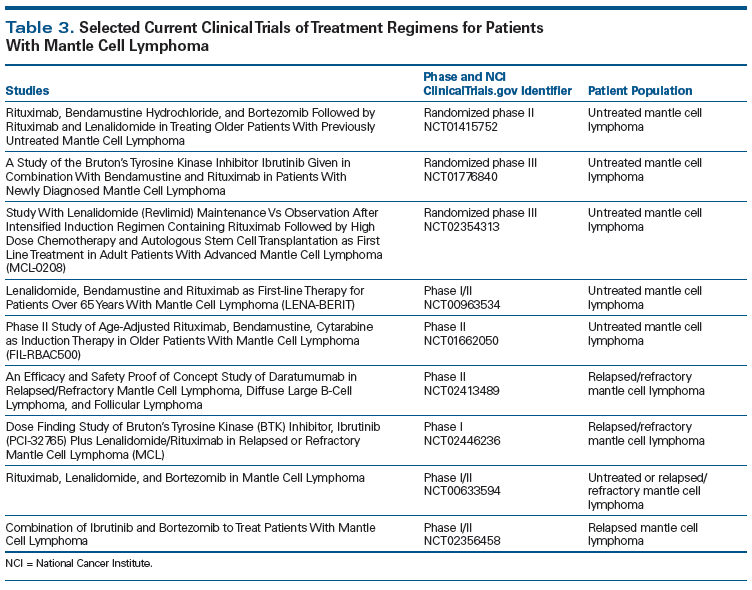
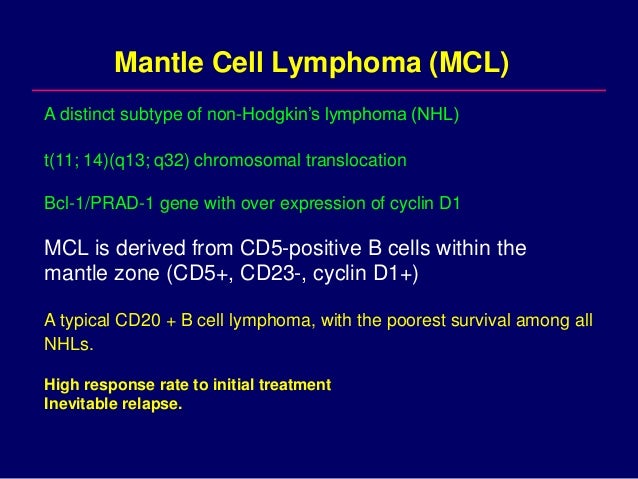
Treatment of mantle cell lymphoma in older adults - Journal of Geriatric Oncology© 2021 MJH Life Sciences and Cure Today. All rights reserved. © 2021 MJH Life SciencesTM and Cure Today. All rights reserved. Advances in the treatment of mantle cell lymphoma are significantly improving the long-term perspective for patientsCURE Exciting advances in treatment options for patients with mantle cell lymphoma are greatly improving the perspective for long-term remissions. When James Landon received a diagnosis of mantle cell lymphoma (MCL) in 2017, he was told that his disease was "indolent," meaning it was slow growth and did not have to be treated immediately, especially because it felt good. But that changed in 2019. Landon, 50, a lawyer in Tucson, Arizona, started feeling tired all the time. His doctors discovered that his white blood cell count was high and his spleen enlarged. The first-line treatment for LCL has long been high doses of chemotherapy, often followed by a stem cell transplant. But when Landon traveled to the University of Texas MD Anderson CancerCenter in Houston to explore his options, he was offered an alternative: an experimental regime combining Imbruvica (ibrutinib) and Rituxan (rituximab). Imbruvica blocks a protein called Bruton tyrosine kinase (BTK), which is a MCL driver, and Rituxan is an antibody that points to hyperactive B cells of the immune system that have been involved in the disease. Five months after starting the combination—four Imbruvica pills every morning and once a week Rituxan infusions—the Landon postitron emission tomography (PET) showed no evidence of disease. If it remains clear, it will undergo a short course of chemotherapy and then move to a one-year maintenance therapy of Ibrutinib and two of Rituxan. "Having this option has been fantastic, in my opinion, because the drugs have so far worked well for me, without toxicity," says Landon, who adds that he has a lot of energy to work full-time and play with his 10-year-old son. BTK inhibitors and immunotherapy are among the new therapeutic options for LCL patients who are significantly improving the prospect for long-term survival. In addition to these specific drugs, Tecartus (brexucabtagene autoleucel) — the first cell genetic therapy for BMC in patients who have not responded or who have relapsed following other types of treatment — was approved by the Food and Drug Administration (FDA) in July and is a one-time personalized treatment from patients' immune cells. "We now have several good non- chemotherapy options for MCL treatment," says Dr. Anthony Nguyen, professor at the University of Nevada, the Las Vegas School of Medicine and a medical oncologist at the Nevada Comprehensive Cancer Centers. "We can tell patients that we can treat them without toxic chemotherapy, which can be reassuring, especially for older patients." MCL is a non-Hodgkin lymphoma subtype (NHL) that is characterized by overproduction of a protein called a D1 cycline. In about 85% of patients, this overproduction is caused by a genetic abnormality called reciprocal chromosomal translocation, which can be detected with diagnostic tests of tumor samples. MCL represents about 6% of all NHL diagnosis and is more common in men than in women, according to the Leukemia Lymphoma Society. The first-line standard treatment for LCL is high-dose chemotherapy, often with a four-drug regimen called hyper-CVAD, followed by a stem cell transplant with a patient's own cells or a donor's. The regime often places patients in long-term referrals, but side effects — including nausea, oral ulcers and kidney damage — can be difficult or even dangerous, especially for patients with other diseases. New medications and cell therapy were approved by the FDA to treat LCL patients who do not respond to chemotherapy and transplants or who fall back. But as doctors get more experience with these therapies, there is a growing interest in using them before in the treatment process to not only improve the possibilities of long-term referrals, but also improve the quality of life of patients by spitting them out of hard side effects. MCL Driver Objective The FDA approved the first BTK inhibitor to treat MCL, Imbruvica, in 2013, based on a study showing a global response rate (which means the disease responded to treatment) of 68% and a full response rate (the disappearance of all signs of cancer) of 21%. The average period that patients lived without their disease progressing was more than a year, and the side effects were mild stomach discomfort and fatigue. The most recently approved BTK inhibitors Calquence (acalabrutinib) and Brukinsa (zanubrutinib) have improved in those response rates. Patients who received Brukinsa in a late trial, for example, had a global response rate of 89 per cent and a full response rate of 59 per cent. Another specific treatment, Venclexta (venetoclax) is also being studied in MCL. Venclexta is directed to BCL2 protein, which promotes cell survival and is abnormally high in MCL — helping to boost disease progression. In a small trial of Venclexta, 75% of patients with relapse LCL responded to the drug, 21% of whom had complete answers. There is even more interest in studying BCL2 inhibition in combination with BTK blockers. In a recent study of Venclexta combined with Imbruvica, the average progression-free survival time was 29 months. "This is a very promising combination," says Dr. Abhijeet Kumar, assistant professor at the hematology and oncology division at the University of Arizona College of Medicine. Kumar is a researcher in an ongoing trial of Venclexta and Imbruvica in MCL. However, there is a risk of increased side effects when specific treatments are combined. Imbruvica can cause bleeding, for example, and both drugs can reduce neutrophil counts (a type of white blood cells). Venclexta is also known for causing tumor lysis syndrome, a rapid release of tumor cells in the bloodstream that can endanger the kidneys and other organs. Still, so far, "the combination seems to be well tolerated," Kumar says. Another treatment of two drugs for the MCL that has generated enthusiasm among the oncologists who treat the disease is called "R-squared" because it combines Rituxan with Revlimid (lenalidomide), a medicine that works by increasing the T cells of the immune system and the natural killer cells, who work together to attack the cancer. In a study of R-squared in 38 newly diagnosed LCL patients, the rate of non-progression survival after three years was 80% and overall survival reached 90%. "The answer is durable," says Dr. Bijal Shah, associate member of the malignant hematology department of the Moffitt Cancer Center and one of the study researchers. During the trial of the R-Table, patients usually stayed in the combination for three years and then took Revlimid only while the disease remained stable. Similar benefits have been seen with a combination of Velcade (bortezomib), Revlimid and chemotherapy, a regimen called VR-CAP. Velcade is a targeted drug that works by altering the growth of MCL cells and encouraging them to die. In a trial of patients with LCL without treatment, adding Velcade to Revlimid and chemotherapy extended the survival without progression by 37%. The addition of Velcade doubled more than the median duration of the response to 41 months. Both R-squared and VR-CAP have moved to the frontline treatment stage, says Shah. "With that, we can see very pronounced clinical benefits. We've seen very long referrals," he says. Other combination strategies for LCL are also being investigated, including some that incorporate Treanda (bendamustine) medication, which works by causing DNA damage to cancer cells. In one study, Treanda's combination with Rituxan improved progression-free survival rates on chemotherapy in patients with painless LMA or NHL. More than 15 studies are currently being conducted that combine Treanda with Rituxan treatments and other MCL treatments. Cell Therapy Charts High Response Rates Although targeted and combined treatments have prolonged survival times in LCL, most patients eventually fell. Now there is a new choice for these patients: Tecartus, a personalized therapy made from a patient's immune cells. The one-time treatment was approved by the FDA to treat patients who have not responded or have declined following other types of treatment. Tecartus is a cymeric antigen receptor (CAR)-T of cell therapy similar to Yescarta (axicabtagena ciloleucel), a CAR-T cell therapy approved by FDA in 2017 to treat some types of large B-cell lymphomas. Like Yescarta, Tecartus points to CD19, a protein that prevails in cancerous B cells. Tecarto is done by extracting T cells from the patient's blood with LMC and genetically modifying those cells to recognize and attack cancer. In addition, cells are placed through a enrichment process designed to prevent them from being used before they are infused again in the patient. In the clinical trial that led to approval, 87 per cent of patients responded to Tecartus and 62 per cent were referred to. Side effects, which included the immune reaction known as cytokine release syndrome and neurological events, were manageable during the clinical trial, says Dr. Michael Wang, a professor of lymphoma and myeloma at the University of Texas MD Anderson Cancer Center and one of the clinical trial researchers. The experience with previously approved CAR-T cell treatments led to widespread use of anti-inflammatory drugs such as interleuken-6 inhibitors and steroids to treat cytokine release syndrome, says Wang. "We have a variety of support measures to manage side effects," he says. With the approval of Tecartus, Wang says that oncologists can imagine a "plant of the survival curve" in MCL. "It's an option for people who become resistant to selective therapies and chemotherapy," he says. "It is very possible that we can put some people on long-term referrals." Become an informed patientBob Brixner, a 20-year-old MCL survivor, has been observing all new developments with interest. When he received a diagnosis of MCL in 2000, he had no choice but to endure chemotherapy followed by a stem cell transplant with his own cells. When he fell again in 2004, he was prescribed a more intense chemotherapy regimen, followed by a stem cell transplant from an unrelated donor. He is grateful that the second treatment put him in a long-term remission, but he still remembers the brutal side effects, including extreme fatigue and pneumonia combat. "And with the transplants, my immune system didn't return 100%," says Brixner, 70, a retired public school teacher from Chicago. "Today, if I take a cold, instead of last a week, it will last three."Brixner advises all newly diagnosed patients to ask many questions about their treatment options, and to get a second opinion. "I think it's really important to be an informed patient," he says, especially because there are many new options. "Some patients may not have to go through what I did," he says. I'm delighted. Related Content:Related Content: NewsThe future is brighter for triple-negative breast cancerSeeding poisonous relationships from the garden of lifeHow TikTok helped a cancer survivor find connection and communityHow targeted therapies are changing the treatment of breast cancer
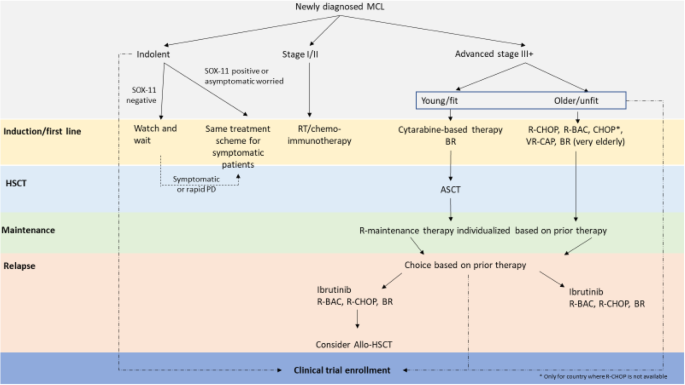
Treatment of mantle cell lymphoma in Asia: a consensus paper from the Asian Lymphoma Study Group | Journal of Hematology & Oncology | Full Text
VA Has More Options as Treatment for Mantle Cell Lymphoma Expands Rapidly - U.S. Medicine

Guideline for the management of mantle cell lymphoma - McKay - 2018 - British Journal of Haematology - Wiley Online Library

Frontline Therapy in Mantle Cell Lymphoma in 2017 | Oncology CME
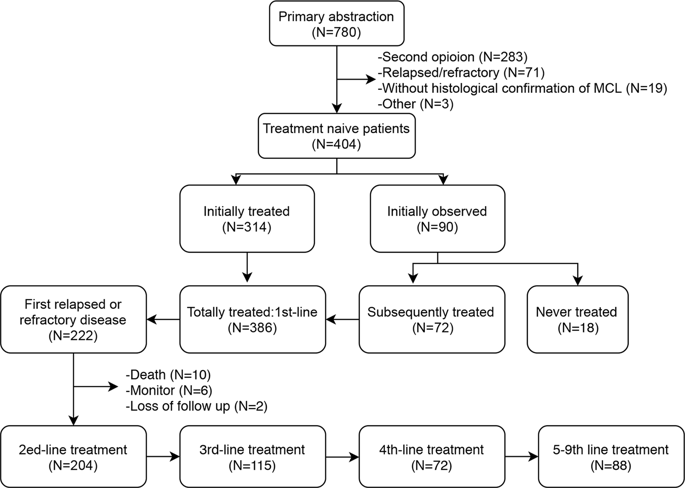
Patterns of survival in patients with recurrent mantle cell lymphoma in the modern era: progressive shortening in response duration and survival after each relapse.,Blood Cancer Journal - X-MOL

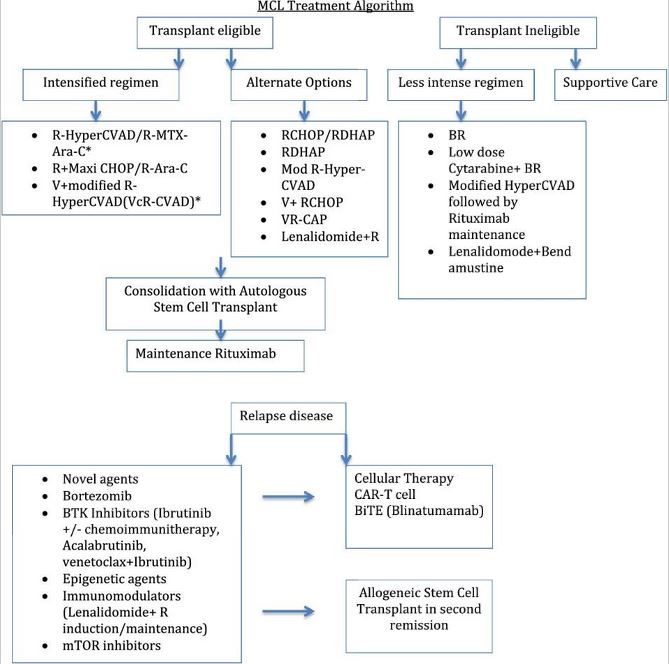
Mantle Cell Lymphoma: Contemporary Diagnostic and Treatment Perspectives in the Age of Personalized Medicine - ScienceDirect
The role of targeted treatment in mantle cell lymphoma: is transplant dead or alive? | Haematologica

Flow diagram of mantle cell lymphoma (MCL) patients receiving frontline... | Download Scientific Diagram
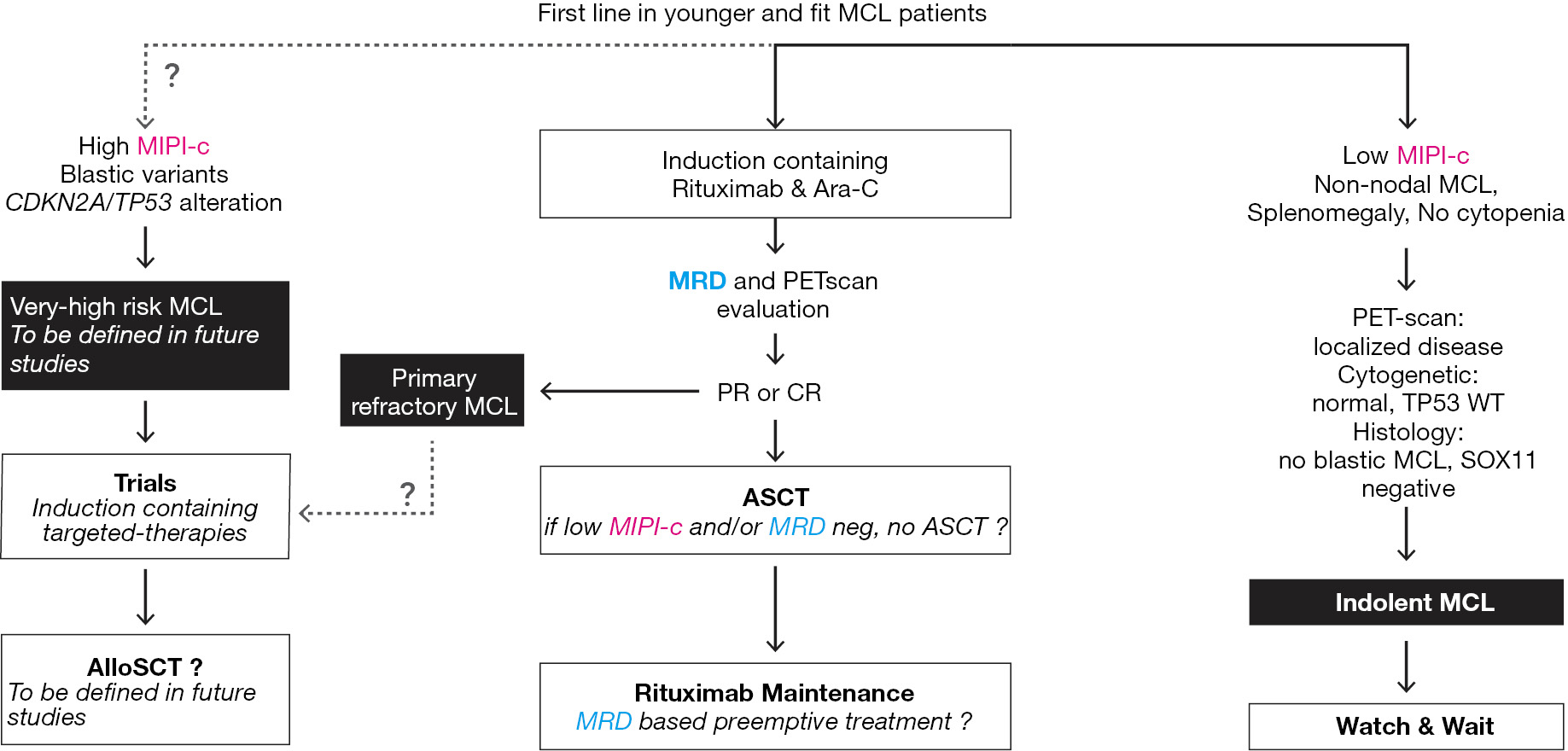
Recent advances in the first-line treatment of mantle cell lymphoma - Cheminant - Annals of Lymphoma

Mantle Cell Lymphoma: Are New Therapies Changing the Standard of Care? - European Medical Journal
Personalized medicine in lymphoma: is it worthwhile? The mantle cell lymphoma experience | Haematologica

Mantle Cell Lymphoma: from bench to clinic

Newly diagnosed and relapsed mantle cell lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up† - Annals of Oncology

Refining the Mantle Cell Lymphoma Paradigm: Impact of Novel Therapies on Current Practice | Clinical Cancer Research

Mantle Cell Lymphoma: Are New Therapies Changing the Standard of Care? - European Medical Journal

Leukemic Non-nodal Mantle Cell Lymphoma: Diagnosis and Treatment | Semantic Scholar

Ibrutinib versus temsirolimus in patients with relapsed or refractory mantle -cell lymphoma: an international, randomised, open-label, phase 3 study - The Lancet

Management of relapsed and refractory mantle cell lymphoma: a review of current evidence and future directions for research - Bond - Annals of Lymphoma

Early clinical trial supports tumor cell-based vaccine for mantle cell lymphoma | EurekAlert! Science News

New Strategies in the Treatment of Mantle Cell Lymphoma | Clinical Cancer Research
Treatment for patients with relapsed/refractory mantle cell lymphoma: European-based recommendations
Mantle Cell Lymphoma Stages and Treatments

Lenalidomide maintenance after autologous haematopoietic stem-cell transplantation in mantle cell lymphoma: results of a Fondazione Italiana Linfomi (FIL) multicentre, randomised, phase 3 trial - The Lancet Haematology
Rituximab after Transplantation in Mantle-Cell Lymphoma | NEJM Resident 360
Clinical Management Updates in Mantle Cell Lymphoma

How to manage mantle cell lymphoma | Leukemia
The role of targeted treatment in mantle cell lymphoma: is transplant dead or alive? | Haematologica

First-line therapy with ASCT in patients with mantle cell... | Download Table

A Systematic Review of Treatments of Relapsed/Refractory Mantle Cell Lymphoma - ScienceDirect

Mantle cell lymphoma – Current standards of care and future directions - Cancer Treatment Reviews

Mantle Cell Lymphoma Treatment Market Growth Forecast from 2020 to 2026 | Worldwide Industry Analysis Focus On business players, Size, Share, Trends, Advanced and Innovative Technology, effective diagnostic solutions and Forecast | Medgadget

Differences in Quality of Life Between Bendamustine-Rituximab and R-CHOP/R-CVP in Patients With Previously Untreated Advanced Indolent Non-Hodgkin Lymphoma or Mantle Cell Lymphoma - Clinical Lymphoma, Myeloma and Leukemia
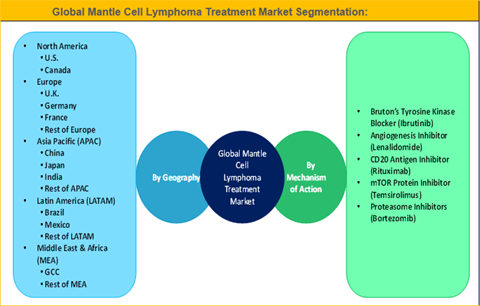
Mantle Cell Lymphoma Treatment Market Size And Forecast To 2025

Mantle cell lymphoma-management in evolution - Rajguru - Chinese Clinical Oncology
Mantle Cell Lymphoma: from bench to clinic

Ibrutinib, lenalidomide, and rituximab in relapsed or refractory mantle cell lymphoma (PHILEMON): a multicentre, open-label, single-arm, phase 2 trial - The Lancet Haematology

Genetic Profiling May Help Treat Mantle Cell Lymphoma | Patient Power
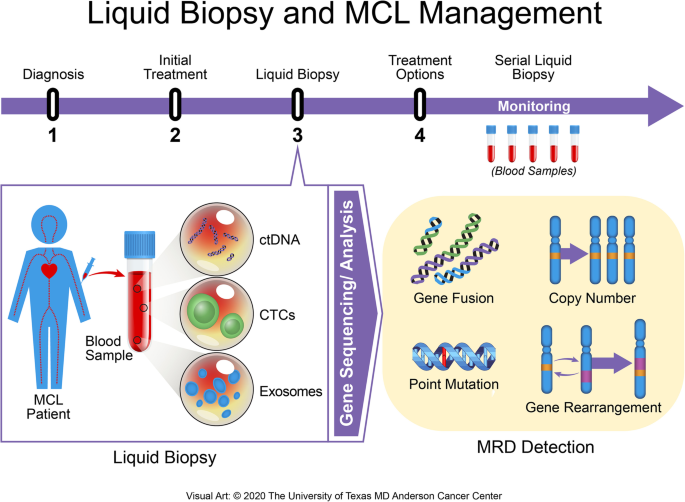
Advances in the assessment of minimal residual disease in mantle cell lymphoma | Journal of Hematology & Oncology | Full Text

Emerging Therapy for the Treatment of Mantle Cell Lymphoma in: Journal of the National Comprehensive Cancer Network Volume 12 Issue 9 (2014)
Posting Komentar untuk "mantle cell lymphoma treatment"